How To Write Soap Note How To Write Soap Note
Best Practices Problemoriented Medical Record And Soap
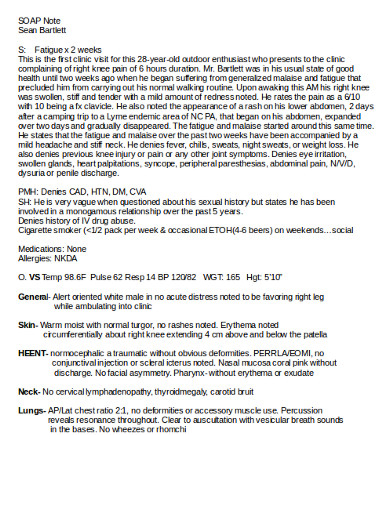
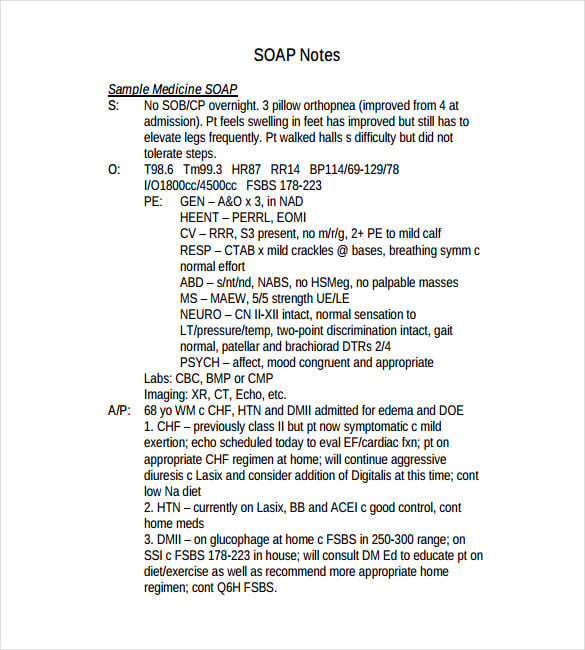
Soap notes are used so staff can write down critical information concerning a patient in a clear, organized, and quick way. soap notes, once written, are most commonly found in a patient’s chart or electronic medical records. to see what a soap note template looks like, check out (and use! ) this example from process street:.
Soap finds its usage soap notes in medical records in recording patient progress. soap or soap notes as they are widely called also find extensive usage in veterinary practices. it is a way for clinics to record, document, and store patient’s medical information in a systematic way. it also gives the practice a framework to evaluate information without losing even the. Soap notes (subjective, objective, assessment, plan) although only one component of the entire pomr have become the standard in clinical record keeping for daily chart notes in ambulatory settings.
Get Latest Info
A medical soap note is written to report on the patient’s current status for further evaluation. this will also help determine whether the mother has made any progress or regress after a specified period. 3. medical examinee soap note. Intuitive charting with flexible templates, efficient e-prescribe, integrated billing. we provide intuitive charting with flexible templates and efficient e-prescriptions. A soap note can be considered to be a progress note containing specific information in a specific kind of format. this is done to help gather up all the important and essential information from a session that will be useful. it’s vital to keep soap notes as part of medical records, especially since it can be how a claim becomes generated.
Soap notes were developed by dr. lawrence weed in the 1960's at the university of vermont as part of the problem-orientated medical record (pomr). each soap note would be associated with one of the problems identified by the primary physician, and so formed only one part of the documentation process. however, various disciplines began using only the "soap" aspect of the format, the "pomr" was. Soap notes are commonly found in electronic medical records (emr) and are used by providers of various backgrounds. generally, soap notes are used as a template to guide the information that physicians add to a patient's emr. [2].
Free Patient Portal
We spoke to doctors who still use paper medical records to learn what the biggest disadvantages of manual systems are. for free software advice, call us now! 855-998-8505 by: lisa hedges on january 7, 2020 since the hitech act passed a deca. The problem oriented medical record and the “academic” soap the goals of the problem oriented medical record (pomr): the pomr is an instructional tool for teaching both medicine and clinical problem solving skills. it is also a useful template for writing medical records for any case that has more than one major problem. The soap note stands for subjective, objective, assessment, and plan. this note is widely used in medical industry. doctors and nurses use soap note to document and record the patient’s condition and status. the soap note is considered as the most effective and standard documentation soap notes in medical records used in the medical industry along with the progress note. Some medical practices may want the fully-written soap note to be reviewed and/or approved by a higher-up, while some practices will want the soap note writer to upload the completed document to a database of medical records. or, the best plan of action may be to carry out the action tasks in the plan as soon as possible.
Soap notes were developed by dr. lawrence weed in the 1960's at the university of vermont as part of the problem-orientated medical record (pomr). each soap note would be associated with one of the problems identified by the primary physician, and so formed only one part of the documentation process. Chart providing details of maine medical records laws internet explorer 11 is no longer supported. we recommend using google chrome, firefox, or microsoft edge. are you a legal professional? visit our professional site » created by findlaw'. A propublica report found more than 180 servers on which people’s medical records were available with minimal or no safeguards. an award-winning team of journalists, designers, and videographers who tell brand stories through fast company's.
Updated Info
A hacker claims to have stolen just shy of 10 million records, and is putting them on for sale on the dark web for about $820,000. the hacker posted the records on the site therealdeal, and the data includes social security numbers, address. A soap note is information about the patient, which is written or presented in a specific order, which includes certain components. soap notes are used for admission notes, medical histories and other documents in a patient’s chart. many hospitals use electronic medical records, which often have templates that plug information into a soap note format. most healthcare clinicians including. Search for how to write soap note. now specific results from your searches! find how to write soap note. search for relevant results here!. Documenting a patient assessment in the notes is something all medical students need soap notes in medical records to practice. this guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your documentation in a clear and consistent manner.

As a therapist, there’s a variety of reasons why you want to take thorough subjective, objective, assessment and planning (soap) notes. you’ll be taking notes for a client’s electronic health record (ehr), which other healthcare providers w. A soap note template comes in a very structured format though it is only one of the numerous formats health or medical professionals can use. a soap note template by a nurse practitioner or any other person who works with the patient enters it into the patient’s medical records in order to update them. Whether you're interested in reviewing information doctors have collected about you or you need to verify a specific component of a past treatment, it can be important to gain access to your medical records online. this guide shows you how.
Huge sale on soap notes examples now on. hurry limited offer. save now!. Confidential patient medical records are protected by our privacy guidelines. patients or representatives with power of attorney can authorize release of these documents. we are experiencing extremely high soap notes in medical records call volume related to covid-19 va.
Each time you hop up on a doctor's exam table, somebody makes a note in your medical records. there may come a time when you need soap notes in medical records your medical information, so find out how to get it and how it's protected. each time you climb up on a doctor. The add new screen allows you to enter a new listing into your personal medical events record. an official website of the united states government the. gov means it’s official. federal government websites always use a. gov or. mil domain. b. It’s a patient’s right to view his or her medical records, receive copies of them and obtain a summary of the care he or she received. the process for doing so is straightforward. when you use the following guidelines, you can learn how to.
The level and complexity of record keeping that you complete will vary according to the context of the intervention and the background health status of your client. the notes a physiotherapist chooses to keep for a patient attending a pilates class will more basic than for example a patient who has had a fall and has a complex medical history. Search for results at top10answers. find your search here.